Gum Disease Treatment That Heals, Not Just Masks
Dec 18, 2025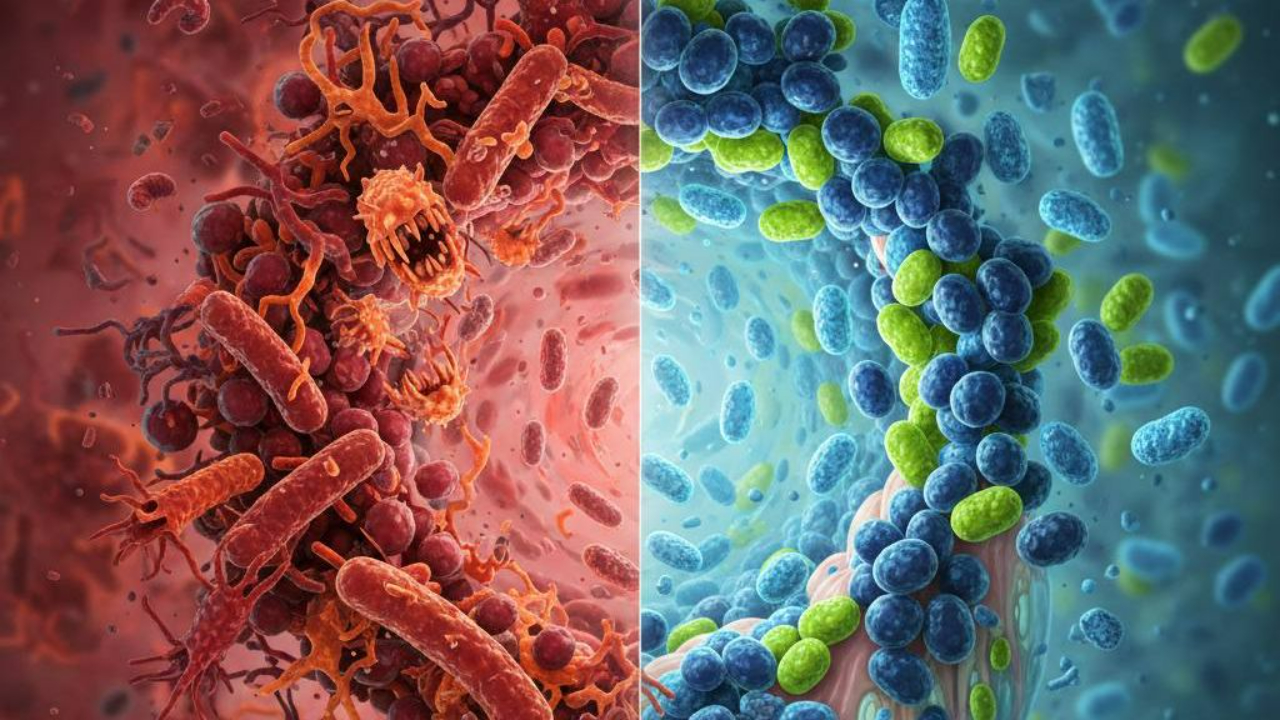
Conventional gum disease treatment only masks the problem — here's how to actually heal your oral microbiome
If you've been through professional cleanings, improved your brushing and flossing, maybe even tried prescription mouthwashes, yet your gums still bleed — you're not alone.
Conventional gum disease treatment focuses on removing bacteria without addressing why those bacteria became problematic in the first place.
In my 18+ years as a dentist and through my work with patients in our oral health program, I've seen this pattern repeatedly:
People do everything their dentist recommends, only to watch their gum problems return within months.
When we shift from fighting bacteria to restoring balance in the oral microbiome, everything changes.
You'll discover why standard treatments fall short, what's really driving your gum inflammation, and how functional dentistry addresses root causes.
You'll also learn about natural protocols that support long-term healing and why testing your oral microbiome might be the breakthrough you've been missing.
Key Takeaways
- Periodontitis is a bacterial imbalance issue, not just an infection⁴, ⁵ — treating it requires restoring microbial balance, not just eliminating bacteria.
- Conventional treatments work short-term but often fail long-term because they don't address nutrient deficiencies, systemic inflammation, or oral microbiome dysbiosis.
- Your oral microbiome contains approximately 700 bacterial species that need to be in proper balance, not eradicated.¹
- Functional dentistry combines professional care with microbiome restoration through targeted nutrition, oral probiotics, and immune support.
- Natural gum disease treatment includes specific nutrients⁶, ⁷, ¹⁵, ¹⁶ like vitamin D, CoQ10, and omega-3 fatty acids that support tissue healing and reduce inflammation.
- Testing reveals your unique bacterial imbalance — what works for someone else may not address your specific oral microbiome issues.
- The mouth-body connection means gum disease affects more than your teeth — it's linked to heart disease, diabetes, Alzheimer's, and systemic inflammation²,³.
Discover the Oral-Systemic Connections
That Could Be Affecting Your Health
Watch the Gateway to Health documentary series FREE for 10 days to understand how your mouth impacts your entire body.
Why your cleanings aren't enough
Traditional dental care excels at what it's designed to do: mechanically remove plaque buildup and bacterial biofilm from tooth surfaces.
Scaling and root planing removes bacteria from below the gum line. This is important work, and it's often necessary.
But here's the critical gap: your mouth is home to approximately 700 different bacterial species,¹ and the goal is not to eliminate them all.
🦠 Your Oral Microbiome: A Complex Ecosystem
Beneficial Bacteria
Protect against infection, support immune function, maintain healthy pH balance
Neutral/Commensal Bacteria
Neither harmful nor helpful — become problematic only when the ecosystem is disrupted
Pathogenic Bacteria
Cause problems when overgrown — drive inflammation, tissue damage, and systemic disease
The goal isn't elimination — it's restoring balance
A healthy oral microbiome requires the right balance of beneficial and pathogenic bacteria.
When treatment focuses solely on reduction rather than restoration, we're bulldozing an entire ecosystem without rebuilding it properly.
Periodontitis doesn't just happen because "bad" bacteria are present — it happens when the microbial community shifts out of balance (what researchers call "dysbiosis"), and your body's inflammatory response becomes chronic and destructive.⁵
If your garden is overrun with weeds, you can pull them out, but if the soil conditions remain unchanged, they'll just grow back.
Want to See Exactly Which Bacteria
Are Out of Balance in Your Mouth?
Our comprehensive oral microbiome testing reveals your unique bacterial profile and creates a personalized protocol to restore balance.
The root causes conventional dentistry often overlooks
After working with hundreds of patients struggling with recurring gum disease, I've identified patterns that standard dental protocols rarely address:
Nutrient deficiencies that feed inflammation
Your gums require specific nutrients to maintain integrity and fight infection.
Vitamin D deficiency has emerged as a significant risk factor for periodontitis,⁶ helping your oral tissues produce antimicrobial peptides.
Antioxidants like CoQ10, vitamins C and E, and omega-3 fatty acids reduce oxidative stress and support tissue repair.⁷
I've seen bleeding gums dramatically improve simply by addressing vitamin D deficiency — changes that's probably never discussed in conventional dental visits.
Systemic inflammation creating oral inflammation
The connection between your mouth and the rest of your body runs both ways.
Systemic inflammation from diabetes, obesity, or chronic stress manifests in your gums.⁸
People with diabetes have 2-3 times higher risk of developing periodontitis.⁹
Immune dysfunction, not just immune response
The tissue destruction comes primarily from your immune system, not directly from the bacteria.¹⁰
When your oral microbiome becomes imbalanced, your immune response can become excessive and chronic, destroying the tissues it's trying to protect.
This explains why two people with similar bacterial profiles can have completely different outcomes.
What's Really Driving Your Gum Disease?
The hidden factors conventional dentistry rarely addresses
Nutrient Deficiencies
Vitamin D helps produce antimicrobial peptides
CoQ10, Vitamin C, E & Omega-3s reduce oxidative stress
Systemic Inflammation
Inflammation from diabetes, obesity, or chronic stress manifests in your gums
People with diabetes have 2-3x higher risk of periodontitis
Immune Dysfunction
Your immune response — not just bacteria — destroys gum tissue
When dysregulated, it attacks the tissues it should protect
Gut-Oral Axis
Gut dysbiosis affects oral health through immune signaling and bacterial translocation
💡 Addressing these factors creates lasting healing — not just temporary relief
How functional dentistry approaches healing differently
Functional dentistry doesn't reject conventional treatments — professional cleanings and surgical interventions have their place.
But we add the critical missing piece: restoring the underlying conditions that support long-term oral health.
The microbiome restoration protocol
Instead of viewing all oral bacteria as enemies, we create an environment where beneficial bacteria can thrive:
Oral probiotics — specific strains like Lactobacillus reuteri and Lactobacillus brevis have shown promise in clinical studies for reducing gingival inflammation and improving periodontal outcomes when used alongside conventional treatment.¹¹,¹²
pH optimization — your oral pH dramatically affects which bacteria flourish.
By addressing dietary factors that create acidic conditions and supporting saliva production, we create a less hospitable environment for pathogenic bacteria.
Biofilm disruption through natural compounds — certain natural substances help break down bacterial biofilms more gently than harsh antimicrobials.
Targeted nutritional support
Based on testing and individual needs, I recommend specific nutrients:
- Vitamin D3 (typically 2000-5000 IU daily) to modulate immune response⁶
- Omega-3 fatty acids to reduce inflammatory mediators⁷
- Coenzyme Q10¹⁵ to reduce gingival inflammation and support periodontal healing
- Antioxidants⁷, ¹⁶ including vitamins C, E, and polyphenols to protect tissues from inflammatory damage
These aren't generic supplements — they're chosen based on your specific inflammatory markers and deficiencies revealed through comprehensive testing.
Addressing systemic contributors
We look at the oral-gut axis connection, blood sugar regulation, stress and sleep, and toxic burden — all factors that directly impact immune function and inflammatory responses.
CTA 3 Preview
Discover How the Gateway to Health Series
Explores These Interconnections in Depth
Watch it FREE for 10 days to understand how your oral health affects your entire body.
What natural gum disease treatment actually looks like
When patients ask me about reversing gum disease naturally, I set realistic expectations.
If you have deep periodontal pockets and significant bone loss, you need clinical intervention.
But natural approaches can be remarkably effective as part of a comprehensive protocol:
Phase 1: Clinical foundation (Weeks 1-4) — Thorough scaling and root planing to remove calculus and smooth root surfaces.
Phase 2: Microbiome restoration (Months 1-3) — Oral probiotic supplementation, targeted nutritional support, optimized oral hygiene, and addressing systemic inflammation.
Phase 3: Maintenance (Ongoing) — Continue supportive nutrients, regular microbiome monitoring, professional cleanings, and lifestyle modifications.
The patients who see the best results understand this isn't a quick fix — it's a fundamental shift in supporting oral health.
The testing advantage most people don't know about
One of the most powerful tools we use in functional dentistry is comprehensive oral microbiome testing.
Instead of guessing which bacteria are causing problems, we can see exactly what's happening in your mouth.
Modern oral microbiome testing identifies specific pathogenic bacteria like Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola — bacteria strongly associated with periodontal disease.¹³
More importantly, it reveals the overall balance and diversity of your oral microbial community, allowing us to create truly personalized protocols.
Get Tested to Stop Guessing and Start Healing
Our Orobiome Testing Package includes:
Comprehensive bacterial analysis of your unique oral microbiome
Consultation with licensed oral health professional
Personalized healing protocol based on YOUR results
What makes holistic periodontal treatment different
Holistic periodontal treatment is grounded in understanding the scientific connections between your mouth and your overall health.
When we address gum disease holistically, we're acknowledging what research has shown for years: periodontal disease is linked to cardiovascular disease, diabetes, Alzheimer's disease, and systemic inflammation.²,³,¹⁴
This doesn't mean abandoning dental care — it means expanding it to ask questions like:
- What's happening in your gut microbiome?
- How well is your immune system functioning?
- Are you getting restorative sleep?
These questions might seem far removed from your bleeding gums, but they're intimately connected to your ability to heal and maintain that healing long-term.
How Gum Disease Affects Your Entire Body
The bidirectional connections between your mouth and systemic health
Your Mouth: The Gateway
Where bacteria enter your bloodstream
Cardiovascular Disease
Oral bacteria enter bloodstream → inflammation in arteries2
2-3x increased risk of heart disease with periodontitis
Alzheimer's Disease
P. gingivalis found in Alzheimer's brains → neuroinflammation14
Direct bacterial pathway from mouth to brain
Diabetes Connection
Bidirectional: gum disease worsens blood sugar control9
High blood sugar feeds pathogenic bacteria
Systemic Inflammation
Chronic oral inflammation elevates whole-body inflammatory markers8
Impacts immune function, energy, and disease risk
🎯 Your gums don't exist in isolation — they're intimately connected to your overall health
Your next steps toward lasting gum health
If you've tried the conventional route and found it wanting, you have options beyond the endless cycle of cleanings and temporary improvements.
Start with testing. Comprehensive oral microbiome testing gives you the roadmap for personalized healing.
Address the foundations. Optimize nutrition, manage stress, and ensure quality sleep — these aren't peripheral concerns, they're central to healing.
Work with practitioners who understand the connections. A functional dentist, biological dentist, or health coach trained in the oral-systemic relationship can see the bigger picture.
Be patient but persistent. You're rebuilding an entire ecosystem. The results tend to be much more stable and lasting than conventional treatments alone.
Moving beyond symptom management
The difference between conventional gum disease treatment and functional approaches comes down to this: one manages symptoms while the other addresses causes.
Both have value, but if you want lasting results, you need to go deeper than the surface.
Your bleeding gums aren't a deficiency of professional cleanings or antibiotics.
They're a signal that something in your oral ecosystem has gone out of balance — and very likely, that imbalance reflects what's happening elsewhere in your body.
The path forward isn't about fighting harder against bacteria.
It's about creating the conditions where your oral microbiome can self-regulate, where your immune system can respond appropriately, and where your gum tissue has the nutritional support it needs to heal and stay healthy.
Ready to Discover What's REALLY Happening
In Your Mouth?
Our Orobiome Test package reveals your unique bacterial profile and creates a personalized protocol for lasting oral health.
Stop masking symptoms and start healing from the root.
Sources
- Periodontal Disease: The Good, The Bad, and The Unknown. Frontiers in Cellular and Infection Microbiology. 2021.
- Local and systemic mechanisms linking periodontal disease and inflammatory comorbidities. Nat Rev Immunol. 2021.
- Association between periodontal pathogens and systemic disease. Biomed J. 2019.
- Periodontal Disease. StatPearls [Internet]. Updated May 12, 2025.
- Dysbiosis revisited. Understanding the role of the oral microbiome in the pathogenesis of gingivitis and periodontitis: A critical assessment. Journal of Periodontology. 2022.
- Vitamin D3 Modulates Inflammatory and Antimicrobial Responses in Oral Epithelial Cells Exposed to Periodontitis-Associated Bacteria. Int J Mol Sci. 2025.
- A cross-talk between diet and the oral microbiome: balance of nutrition on inflammation and immune system's response during periodontitis. Nutrients. 2022.
- Periodontal Inflammation and Systemic Diseases: An Overview. Frontiers in Physiology. 2021.
- Oral microbiota in human systematic diseases. Int J Oral Sci. 2022.
- Host modulation and treatment of periodontal disease. J Dent Res. 2021.
- Probiotics in the non-surgical treatment of periodontitis: a systematic review and network meta-analysis. BMC Oral Health. 2024.
- The Clinical, Microbiological, and Immunological Effects of Probiotic Supplementation on Prevention and Treatment of Periodontal Diseases: A Systematic Review and Meta-Analysis. Nutrients. 2022.
- Risk Factors of Periodontal Disease: Review of the Literature. Int J Dent. 2014.
- Porphyromonas gingivalis in Alzheimer's disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Sci Adv. 2019.
- Clinical efficacy of adjunctive use of coenzyme Q10 in non-surgical periodontal treatment: A systematic review. European Journal of Oral Sciences. 2025.
- Vitamin intake and periodontal disease: a meta-analysis of observational studies. BMC Oral Health. 2024.
Gateway to Health is the new health & wellness division of The Urban Monk. We've moved the health and life sciences content here and are leaving the personal development and mindfulness materials on theurbanmonk.com.
Disclaimer: This content is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Please consult a qualified healthcare professional before making changes to your health protocol.