Gut Testing for Anxiety Proves It's Not All in Your Head
Dec 30, 2025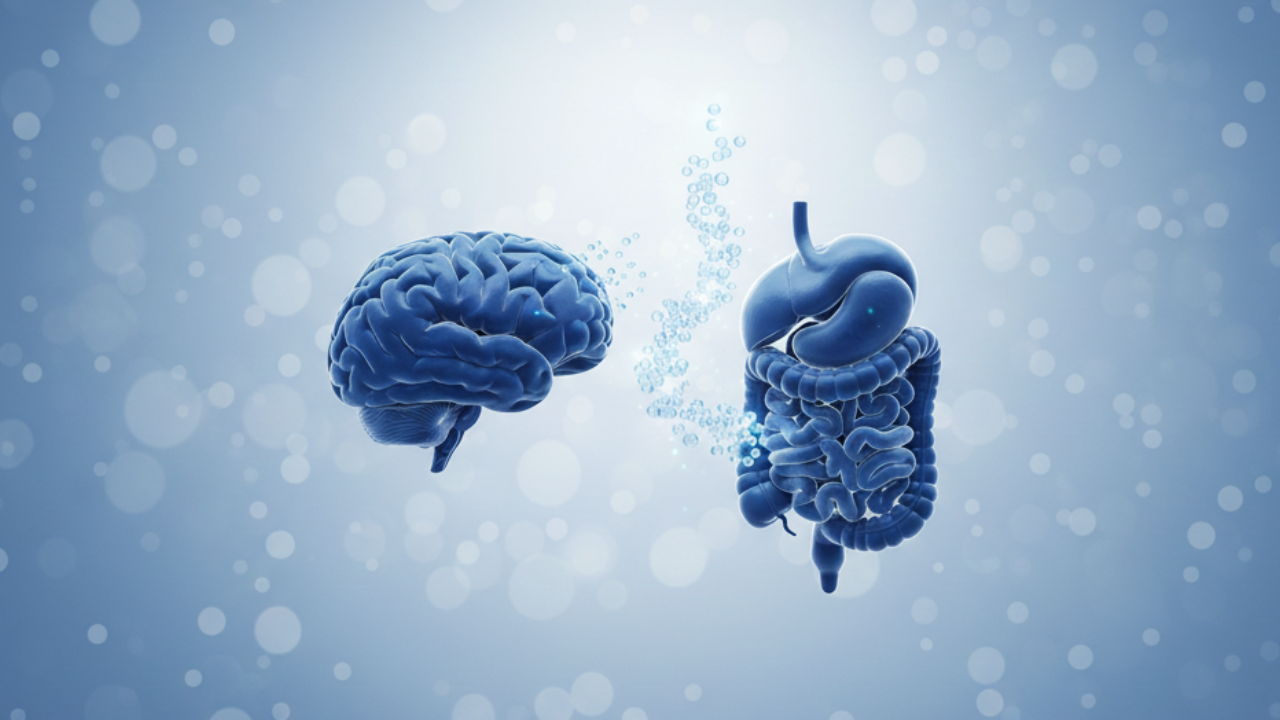
Gut testing for anxiety makes sense when 90% of your serotonin is actually made in your gut
You've tried everything. Years of SSRIs, therapy sessions twice a week, meditation apps, and expensive supplements. You've read every anxiety self-help book on the market.
Yet here you are — still anxious, still struggling, and increasingly frustrated that nothing seems to create lasting change.
Here's what your psychiatrist probably hasn't told you: 90% of your body's serotonin isn't made in your brain at all — it's produced in your gut.¹
And when your gut is inflamed, imbalanced, or compromised, your anxiety might have less to do with your mindset and everything to do with what's happening in your digestive tract.
In this article, you'll discover why gut testing for anxiety is emerging as a critical diagnostic tool that conventional psychiatry often overlooks.
We'll explore the science behind the gut-brain axis, reveal what comprehensive testing can show you about your unique biochemistry, and explain why healing your gut might be the breakthrough you've been searching for.
If you've been told your anxiety is "all in your head" but suspect something deeper is going on, keep reading.
The answers might be closer than you think — specifically, about 2 feet below your brain.
Key Takeaways
- 90% of serotonin is produced in the gut, not the brain¹,³ — making gut health directly connected to mood regulation and anxiety levels.
- The vagus nerve creates a direct communication highway between your gut and brain, transmitting signals that influence emotional states and stress responses²,¹⁰.
- Specific bacteria produce calming neurotransmitters like GABA while other pathogens trigger inflammation that manifests as anxiety⁶,⁷.
- Comprehensive gut testing reveals what generic treatments miss — identifying food sensitivities, bacterial imbalances, and gut barrier breakdown that fuel anxiety.
- Pathogenic oral bacteria swallowed daily can disrupt gut-brain axis function¹³,¹⁴, making oral microbiome testing an important part of anxiety root-cause investigation.
- Gut healing often resolves medication-resistant anxiety when the root cause is inflammation, dysbiosis, or intestinal permeability.
- Testing replaces guessing with personalized data showing exactly which imbalances drive your specific anxiety symptoms.
Understanding What's Happening in Your Gut Is the First Step
Discover what comprehensive testing reveals about YOUR anxiety — includes personalized protocol and consultation.
The Gut-Brain Connection Your Doctor Probably Didn't Mention
In my practice, I've seen it countless times: patients who've spent thousands on psychiatric care, tried six different medications, and still wake up with that familiar knot of anxiety in their chest.
The conversation usually starts the same way: "My doctor says I just need to find the right medication dose."
But here's what conventional psychiatry often misses: your gut and brain are in constant communication through a biological superhighway called the vagus nerve.²
This nerve sends signals in both directions, meaning what happens in your gut directly affects your brain — and your anxiety levels.
Think about it this way: when you're nervous, you feel it in your stomach. When you're stressed, your digestion shuts down. This isn't coincidence.
It's your gut-brain axis in action.
The problem starts when this communication system gets hijacked by inflammation, bacterial imbalances, or a compromised gut barrier.
Suddenly, instead of sending calming signals, your gut is flooding your brain with inflammatory messages that trigger and amplify anxiety.
See the Gut-Brain Axis in Action
Watch our FREE limited-time screening of the Interconnected documentary series and discover how your body's systems work together.
Why 90% of Your Serotonin Lives in Your Gut
Serotonin has long been called the "happiness neurotransmitter." Most people assume it's primarily a brain chemical. Research shows otherwise.
Approximately 90% of your body's serotonin is actually produced by specialized cells in your gut called enterochromaffin cells.¹,³
These cells depend on your gut bacteria to help manufacture serotonin — which means your microbiome directly influences your mood and anxiety levels.
Studies from institutions like Caltech and UCLA have demonstrated that when mice lack specific gut bacteria, their serotonin levels drop by more than 50%.⁴,⁵
Add those bacteria back, and serotonin normalizes. This isn't theoretical — it's measurable, repeatable science.
In humans, the implications are profound.
If your gut bacteria are out of balance — a condition called dysbiosis — your ability to produce adequate serotonin is compromised.
No amount of SSRIs can fix a problem that originates in your digestive tract rather than your brain.
This is where gut testing for anxiety becomes invaluable.
Instead of guessing whether your gut might be involved, comprehensive testing shows you exactly what's happening in your unique microbiome.
What's Disrupting YOUR Serotonin Production?
Testing reveals gut barrier breakdown, bacterial overgrowth, and toxins that disrupt your microbiome and interfere with serotonin production.
The GABA Connection: Your Gut's Calming Chemistry
Serotonin isn't the only neurotransmitter your gut influences.
GABA (gamma-aminobutyric acid) is your brain's primary calming neurotransmitter — the chemical that helps you feel relaxed, sleep well, and maintain emotional balance.
Groundbreaking research from Northeastern University discovered that certain gut bacteria are the primary producers of GABA in your body.⁶,⁷,⁸
More importantly, they found that people with depression and anxiety have significantly lower levels of these GABA-producing bacteria, particularly species of Bacteroides.⁸
The researchers used functional MRI brain scans to confirm the connection: lower levels of GABA-producing bacteria correlated directly with brain patterns associated with depression and anxiety.⁸
What makes this discovery so significant is that it explains why some people's anxiety doesn't respond to conventional treatment.
If you're lacking the gut bacteria that produce calming neurotransmitters, medication targeting brain chemistry alone will always fall short.
I've worked with patients who tested low in Lactobacillus and Bifidobacterium species — both known GABA producers — and struggled with treatment-resistant anxiety for years.
When we addressed their gut dysbiosis through targeted protocols based on testing results, their anxiety improved in ways medication never achieved.
GABA-Producing Bacteria
Your gut bacteria manufacture calming neurotransmitters that regulate anxiety
Primary GABA producer.⁶,⁸ Research shows people with depression and anxiety have significantly lower levels of these beneficial bacteria.⁸
GABA manufacturer via vagus nerve.¹² Studies show specific strains regulate emotional behavior and brain receptor expression.¹²
Supports GABA production.⁶ Essential for maintaining gut-brain communication and reducing anxiety responses.
What GABA Does
GABA is your brain's primary calming neurotransmitter — it helps you feel relaxed, sleep well, and maintain emotional balance. Without adequate GABA-producing bacteria, anxiety persists despite medication.
What Gut Testing Actually Reveals About Your Anxiety
Standard psychiatric evaluation can't see what's happening in your gut.
Blood tests ordered by conventional doctors rarely assess the markers that matter for gut-brain health.
This is why gut testing becomes transformative.
Comprehensive gut testing examines several critical factors that can drive anxiety:
Food Sensitivity Testing (IgG & C3d)
Delayed food reactions create systemic inflammation that directly affects brain function.
Unlike immediate allergies, these sensitivities can trigger anxiety hours or even days after eating trigger foods — making them nearly impossible to identify without testing.
Gut Permeability Markers
Tests measuring Zonulin, Occludin, and LPS (lipopolysaccharide) reveal whether you have "leaky gut" — a condition where your intestinal barrier breaks down, allowing bacterial toxins to enter your bloodstream.
Research shows LPS in the bloodstream creates neuroinflammation that manifests as anxiety, brain fog, and depression.⁹
Bacterial Balance Analysis
Testing identifies which beneficial bacteria you're lacking (like GABA and serotonin producers) and which pathogenic bacteria or yeast overgrowth you're carrying.
This data allows for targeted intervention instead of generic probiotics that may not help your specific situation.
Candida and SIBO Screening
Both Candida overgrowth and Small Intestinal Bacterial Overgrowth (SIBO) are strongly associated with anxiety.
Candida produces neurotoxic byproducts, while SIBO creates fermentation that triggers inflammatory cascades affecting the brain.
What Comprehensive Gut Testing Reveals
Food Sensitivity Analysis
IgG & C3d testing for 22-176 foods identifies delayed inflammatory reactions triggering anxiety symptoms
Gut Barrier Breakdown
Zonulin & Occludin levels show if "leaky gut" is allowing toxins into your bloodstream
Bacterial Toxin Levels
LPS (lipopolysaccharide) measurement reveals inflammation-triggering bacterial toxins in your system
Candida & Bacterial Balance
Candida antibodies and bacterial overgrowth detection uncover hidden dysbiosis affecting mood
💡 Testing replaces guessing — showing exactly which imbalances drive YOUR specific anxiety symptoms
I recently worked with a woman who'd been on anxiety medication for eight years.
Her gut testing revealed severe gluten and dairy sensitivity, elevated Zonulin indicating leaky gut, and candida overgrowth.
Within three months of following her personalized protocol — which included removing trigger foods and healing her gut barrier — her anxiety decreased significantly.
She was able to reduce her medication under her doctor's supervision for the first time in years.
The Vagus Nerve: Your Gut-Brain Information Highway
Understanding the vagus nerve is crucial to understanding why gut health so profoundly affects anxiety.
This cranial nerve is the longest in your body, starting in your brainstem and extending all the way down to your colon.
The vagus nerve serves as the primary communication pathway between your gut and brain, with 80-90% of its fibers carrying information FROM your gut TO your brain — not the other way around.¹⁰,¹¹
This means your gut is constantly sending signals that influence your emotional state, stress response, and even cognitive function.
When your gut is inflamed or imbalanced, the signals traveling up the vagus nerve tell your brain that something is wrong.
Your brain interprets these danger signals as stress or threat, triggering anxiety even when there's no external reason to feel anxious.
Research published in Frontiers in Psychiatry demonstrates that vagal tone — how well your vagus nerve functions — correlates directly with your capacity to regulate stress responses and manage anxiety.²
People with better vagus nerve function experience less anxiety and recover from stress more quickly.
The good news? Improving your gut health improves vagal signaling.
Studies show that specific probiotic strains can enhance vagus nerve activity, creating a positive feedback loop between gut healing and anxiety reduction.¹²
Practices like meditation and specific breathing exercises also strengthen vagus nerve function — which is why combining gut healing with stress reduction techniques creates synergistic benefits.
Learn proven vagus nerve exercises that calm anxiety naturally.
The Vagus Nerve: Your Gut-Brain Information Highway
Brain (Brainstem)
Receives signals about gut status
Vagus Nerve
Longest cranial nerve connecting brain to gut
Gut & Microbiome
Sends signals about inflammation, bacteria balance, and danger
💡 When your gut is inflamed or imbalanced, the vagus nerve sends danger signals to your brain — triggering anxiety even without external threats.
When Conventional Treatment Misses the Mark
Conventional psychiatry typically focuses on neurotransmitter levels in the brain, which is why SSRIs (selective serotonin reuptake inhibitors) are the standard treatment for anxiety.
These medications work by preventing your brain from reabsorbing serotonin, theoretically making more available.
But here's the limitation: if your gut isn't producing adequate serotonin in the first place, or if inflammation is disrupting the gut-brain axis, manipulating brain chemistry alone won't solve the problem.
Additionally, while SSRIs do affect gut microbiota composition, this impact doesn't replace the need to understand your baseline gut health — particularly if you have compromised gut barrier function or pathogenic bacterial colonization that's driving inflammation in the first place.
This isn't to say psychiatric medications don't have value. For some people, they're life-changing.
But for others — particularly those with medication-resistant anxiety — the root cause isn't in the brain at all.
An integrative approach recognizes that both gut health and brain chemistry matter.
When we combine the insights of functional medicine with conventional psychiatry, we create more comprehensive solutions.
The psychiatric medication provides stabilization while we work on gut healing.
As the gut heals and the underlying inflammation resolves, many patients can reduce or discontinue medication under their doctor's supervision.
This isn't an either/or situation.
It's about finding the right approach for your specific situation — which starts with understanding what's actually driving your anxiety.
The Oral Microbiome Connection You're Overlooking
Most people don't realize that the bacteria in your mouth directly affect your gut-brain axis.
Every time you swallow — which happens approximately 2,000 times per day — you're introducing oral bacteria into your digestive system.
When pathogenic oral bacteria make their way to your gut, they can trigger systemic inflammation that affects your brain function and contributes to your anxiety.¹³,¹⁴
The Oral-Gut-Brain Connection
Oral Microbiome
Pathogenic bacteria colonize your mouth
Gut Microbiome
Harmful oral bacteria disrupt gut balance and trigger systemic inflammation¹³,¹⁴
Gut-Brain Axis
Vagus nerve transmits inflammatory signals from gut to brain
Neuroinflammation & Anxiety
Brain inflammation manifests as anxiety, brain fog, and mood disorders¹³,¹⁴
💡 Your oral microbiome affects your anxiety ~2,000 times daily — making oral health testing critical for root-cause investigation.
This is particularly relevant because research shows specific oral pathogens are associated with neuroinflammation and mood disorders.
This connection is why we often recommend oral microbiome testing as part of a comprehensive anxiety investigation — especially if you also have digestive symptoms or a history of gum disease.
Your Mouth Affects Your Gut ~2,000 Times Daily
Explore comprehensive oral microbiome testing to identify hidden inflammation sources that may be driving your anxiety.
Pathogenic oral bacteria can trigger inflammation that reaches your brain.
Your Next Steps: From Testing to Healing
If you recognize yourself in these patterns — anxiety that doesn't fully respond to conventional treatment, digestive issues that seem unrelated, brain fog accompanying your anxiety — gut testing might be your breakthrough.
Here's what a comprehensive gut-testing protocol typically involves:
- Complete Testing Panel: Food sensitivity testing (22-176 foods), gut permeability markers, bacterial balance analysis, and pathogen screening
- Personalized Protocol: Based on your specific results, not generic recommendations
- Professional Guidance: One-on-one consultation to interpret results and create your healing plan
- Root Cause Approach: Addressing what's actually driving your anxiety instead of just managing symptoms
The investment in testing often saves thousands of dollars in treatments that don't work because they're not addressing your specific imbalances.
When Medication Alone Isn't Enough
Find out if gut dysfunction is driving your anxiety. Comprehensive testing reveals your unique imbalances and root causes.
💡 Testing helps you understand what's been missing from your treatment approach.
Final Thoughts
Your anxiety isn't "all in your head" — and you're not imagining the connection between your gut and your mood.
Research from leading institutions confirms what functional medicine practitioners have observed clinically for years: gut health and mental health are inseparably linked.
The question isn't whether your gut affects your anxiety.
The question is: what specifically is happening in YOUR gut that's contributing to YOUR anxiety?
That's what testing reveals. That's what creates the foundation for real, lasting healing.
You've tried the conventional approach. You've given medication and therapy a fair chance. If you're still struggling, your gut might be the variable nobody's addressed yet.
Ready for Real Answers?
Get comprehensive gut testing to uncover what's driving YOUR anxiety—includes personalized consultation and healing protocol.
✓ Comprehensive Testing
✓ Personalized Protocol
✓ Expert Consultation
Sources
- Exploring the serotonin-probiotics-gut health axis: A review of current evidence and potential mechanisms. Food Science & Nutrition. 2023.
- Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Frontiers in Psychiatry. 2018.
- Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell. 2015.
- Study shows how serotonin and a popular anti-depressant affect the gut's microbiota. 2019.
- Microbes Help Produce Serotonin in Gut. Caltech. 2015.
- GABA-modulating bacteria of the human gut microbiota. Nature Microbiology. 2019.
- Newly isolated human gut bacterium reveals possible connection to depression. DOE/Argonne National Laboratory. 2019.
- GABA Modulating Bacteria of the Human Gut Microbiota. Nature Microbiology. 2018.
- Mood disturbance during experimental endotoxemia: Predictors of state anxiety as a psychological component of sickness behavior. Brain, Behavior, and Immunity. 2016.
- The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Frontiers in Neuroscience. 2018.
- Vagus nerve central to the gut-brain axis. UCLA Health. 2025.
- Ingestion of Lactobacillus strain regulates emotional behavior and central GABA receptor expression in a mouse via the vagus nerve. Proceedings of the National Academy of Sciences. 2011.
- Human oral microbiome and its influence on mental health and brain disorders. AIMS Microbiology. 2025.
- The Oral–Gut Microbiota Axis Across the Lifespan: New Insights on a Forgotten Interaction. Nutrients. 2025.
Gateway to Health is the new health & wellness division of The Urban Monk. We've moved the health and life sciences content here and are leaving the personal development and mindfulness materials on theurbanmonk.com.
Disclaimer: This content is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Please consult a qualified healthcare professional before making changes to your health protocol.