Oral Health and Heart Disease: The Warning You Missed
Dec 11, 2025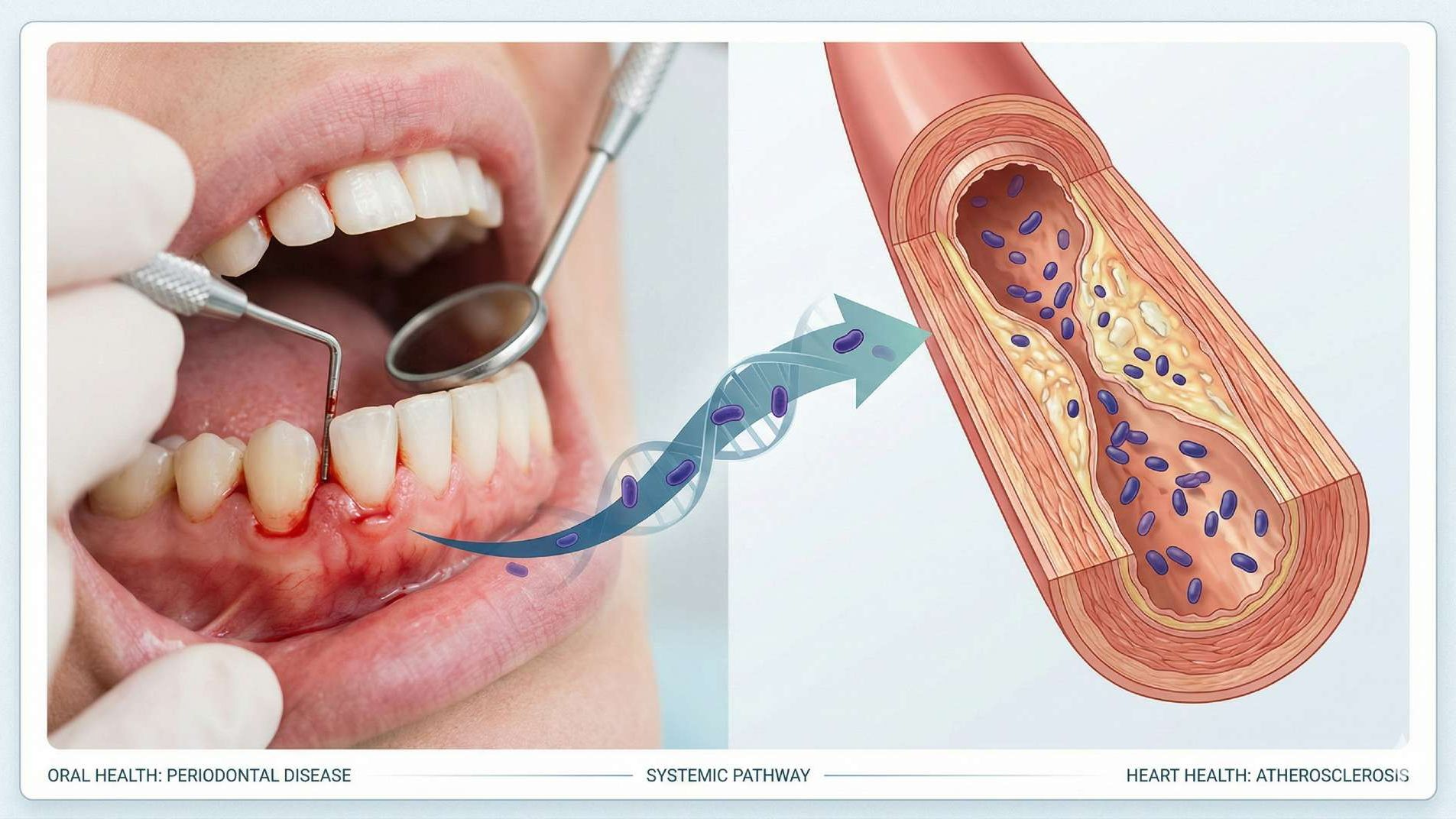
Oral health and heart disease: The critical warning sign your dentist sees that could predict your heart attack
The bacteria in your mouth can travel directly to your heart. Not metaphorically. Not eventually.
Right now, with every swallow, you're sending approximately 100 billion bacteria into your digestive system daily — and when your gums are inflamed, these microbes can enter your bloodstream¹³,¹⁴ — and cardiologists are finally paying attention to what this means for your survival.
I've spent over 18 years as a functional dentist, and I can tell you this: some of the most dangerous warning signs I see have nothing to do with cavities.
When I examine someone's gums and see chronic inflammation, bleeding on contact, or deep periodontal pockets, I'm not just seeing dental problems.
I'm often looking at someone's cardiovascular system sending up distress signals — and most patients have no idea.
In this article, you'll discover the scientifically-proven connection between oral health and heart disease, why conventional dentistry misses these critical warning signs, and most importantly, what you can do right now to protect both your mouth and your heart.
If you've ever wondered why your gums bleed when you floss, or if that "minor" periodontal issue could actually matter, keep reading.
The answers could literally save your life.
Key Takeaways
- Patients with periodontitis exhibit a 1.27-fold higher prevalence of atherosclerosis and have more than double the risk of cardioembolic and thrombotic stroke compared to those with healthy gums.¹,¹⁰
- Porphyromonas gingivalis, a common oral pathogen, has been found colonizing coronary and femoral arteries and actively destabilizes arterial plaque, increasing heart attack risk.²,³,¹⁷
- Bleeding gums trigger a systemic inflammation cascade that elevates C-reactive protein (CRP), a key biomarker for cardiovascular disease risk.⁴,⁷
- The oral-heart connection works both ways: chronic oral inflammation fuels heart disease, while heart disease patients with untreated periodontitis face worse cardiovascular outcomes.⁵
- Younger adults under 50 with periodontitis show a 72% increased risk of coronary heart disease, making early detection critical.¹¹
- Periodontal treatment reduces systemic inflammation markers including CRP levels, potentially lowering cardiovascular disease risk.⁷
- Oral microbiome testing reveals pathogenic bacteria before they cause irreversible damage to both your mouth and your cardiovascular system.
Your Dentist Sees What Your Cardiologist Can't
Here's something most people don't realize:
Your mouth is one of the only places in your body where healthcare providers can visually assess your inflammatory state without invasive procedures.
When I examine gums that bleed easily, show recession, or have deep pockets around the teeth, I'm seeing active, chronic inflammation — the same inflammatory process that damages your arteries.
One of my patients came in for a routine cleaning with textbook "healthy" cholesterol numbers and normal blood pressure.
But her gums told a different story. Moderate periodontitis, consistent bleeding, and visible inflammation.
When I mentioned that her oral health might be signaling cardiovascular risk, she was skeptical.
"My cardiologist said everything looks fine."
Six months later, after getting comprehensive oral microbiome testing, she discovered dangerous levels of Porphyromonas gingivalis — the same pathogenic bacteria researchers have found colonizing the arteries of heart attack victims.²,¹⁷
Her oral health wasn't just a dental issue. It was a cardiovascular time bomb.
The Bacteria Behind Your Bleeding Gums Can Attack Your Heart
Let's talk about Porphyromonas gingivalis (P. gingivalis) — arguably the most dangerous bacteria lurking in diseased gums.
This isn't just speculation.
Researchers have literally found this oral pathogen living inside the atherosclerotic plaques of heart attack victims,²,³ with one major study detecting P. gingivalis as the most abundant bacterial species in coronary and femoral arteries.¹⁷
Here's how it works: P. gingivalis doesn't stay confined to your mouth.
Every time you brush, floss, chew, or even swallow, bacteria from infected gums can enter your bloodstream through tiny tears in your oral tissues — a phenomenon called bacteremia.⁸
Once in circulation, these oral bacteria can invade your arterial walls, where they set up camp and trigger a cascade of damage.
Studies published in Signal Transduction and Targeted Therapy demonstrated that P. gingivalis directly promotes atherosclerotic plaque instability by:¹,²
- Triggering oxidative stress in arterial macrophages
- Promoting foam cell formation (lipid-laden immune cells that form plaque cores)
- Enlarging the necrotic core of existing plaques
- Increasing the likelihood of plaque rupture — the event that causes most heart attacks
Think of it like this: if your arteries are highways, plaque buildup is like potholes forming over time.
P. gingivalis doesn't just create potholes — it actively weakens the road structure until a catastrophic collapse (heart attack) becomes inevitable.
The numbers are sobering.
Patients with periodontitis exhibit a 1.27-fold higher prevalence of atherosclerosis compared to those with healthy gums.¹
And research from the PAROKRANK study found that people with moderate to severe periodontitis have a 28% increased risk of first-time myocardial infarction (OR 1.28, 95% CI 1.03-1.60), even after adjusting for traditional cardiovascular risk factors.⁹
From Bleeding Gums to Damaged Arteries
The connection between gum disease and heart attack isn't just about bacteria traveling to your heart — it's about inflammation.
Chronic periodontitis keeps your immune system in a constant state of low-grade warfare, and that has profound systemic consequences.
When your gums are inflamed, your liver responds by producing C-reactive protein (CRP), an acute-phase inflammatory marker.⁴,⁷
Elevated CRP levels don't just indicate inflammation — they actively participate in cardiovascular damage by:
- Inducing endothelial dysfunction (damage to blood vessel linings)
- Promoting adhesion molecule expression (making plaque stick to artery walls)
- Activating the complement cascade (immune responses that worsen arterial damage)
- Reducing beneficial nitric oxide production (which normally keeps blood vessels healthy)
Multiple studies have confirmed that patients with periodontitis show significantly elevated CRP levels compared to periodontally healthy individuals.⁴,⁷
More importantly, successful periodontal treatment reduces these inflammatory markers — potentially lowering cardiovascular disease risk.⁷
One patient told me, "I thought bleeding gums just meant I needed to floss more."
He wasn't wrong about needing to floss, but he was dramatically underestimating what those bleeding gums signified.
Chronic gum bleeding isn't normal. It's your body waving a red flag that systemic inflammation is out of control.
Learn more about how bleeding gums affect your heart and brain →
The Data Doesn't Lie
Let's look at what large-scale studies tell us about the oral health and heart disease connection:
Prevalence and Risk
A meta-analysis examining over 2.7 million participants found that the pooled prevalence of cardiovascular disease in patients with periodontal disease was 7.2% (95% CI: 2.7-13.6%).⁶
But here's the critical detail:
Younger patients (mean age under 45) with periodontitis showed a dramatically higher CVD prevalence of 23.8% compared to just 7.5% in older adults (mean age 45 or older).⁶
This suggests that periodontal disease may accelerate cardiovascular events in younger individuals who haven't yet developed traditional risk factors.
Additionally, males younger than 50 years of age with periodontitis were 72% more likely to develop coronary heart disease compared to their periodontally healthy counterparts.¹¹
Stroke Risk
Patients with periodontitis have more than double the risk of cardioembolic and thrombotic stroke compared to periodontally healthy individuals.¹⁰
That's not a minor increase — it's a fundamental shift in stroke probability.
Mortality
Two large cohort studies reported that periodontitis is associated with higher cardiovascular mortality due to both coronary heart disease and cerebrovascular disease.¹¹
Having diseased gums doesn't just increase your risk of having a cardiac event — it increases your risk of dying from one.
These aren't correlations we can dismiss.
The American Heart Association recognizes an independent association between periodontal disease and atherosclerotic vascular disease,¹² and research consistently shows that this relationship persists even after controlling for traditional risk factors like smoking, diabetes, and hypertension.
What Your Cardiologist Probably Isn't Telling You
Here's the uncomfortable truth: most cardiologists aren't asking about your oral health.
They're checking your cholesterol, monitoring your blood pressure, maybe prescribing statins — but they're not looking in your mouth.
And most dentists aren't connecting periodontal disease to systemic health outcomes beyond giving you a pamphlet about "the mouth-body connection."
This creates a dangerous gap in preventive care.
I've seen patients with impeccable cardiovascular numbers on paper who have raging oral infections — and vice versa.
The oral-systemic connection isn't theoretical anymore. It's supported by decades of research and hundreds of peer-reviewed studies.
In my practice, when I identify moderate to severe periodontitis, I don't just recommend better brushing or flossing.
I explain that they're dealing with a chronic inflammatory disease that extends far beyond their mouth — one that could be silently damaging their cardiovascular system right now.
Prevention Starts With Knowledge
The good news? Unlike many cardiovascular risk factors, periodontal disease is preventable and treatable.
But you can't treat what you don't know about.
This is where comprehensive oral microbiome testing becomes crucial.
Traditional dental exams can identify periodontal disease through visual inspection and probing depths, but they can't tell you which specific bacterial strains are colonizing your mouth.
Testing reveals:
- Exact pathogenic species present (including P. gingivalis)
- Bacterial load and diversity
- Specific strains associated with cardiovascular risk
- Your unique oral ecosystem profile
With this data, treatment can be targeted rather than generic.
Instead of broad-spectrum antimicrobials that disrupt your entire oral microbiome, you can address specific pathogenic bacteria while preserving beneficial species.
It's precision medicine for your mouth — and potentially for your heart.
Your Mouth as Your Cardiovascular Early Warning System
I often tell patients: your mouth is the most accessible window into your systemic health.
We can see chronic inflammation in action.
We can identify pathogenic bacteria before they cause irreversible damage.
We can intervene early — years before a cardiovascular event might occur.
The research on oral microbiome testing shows that identifying and treating periodontal pathogens reduces systemic inflammatory markers like CRP.⁷
While we need more long-term studies to definitively prove that treating gum disease prevents heart attacks, the mechanistic pathways are clear: reduce oral infection, reduce systemic inflammation, potentially reduce cardiovascular risk.
Think about it this way: if you knew that a simple saliva test could reveal bacteria linked to heart disease — bacteria that are actively circulating in your bloodstream right now — wouldn't you want that information?
Beyond Brushing and Flossing
Standard oral hygiene is important, but it's not enough if you already have established periodontitis or pathogenic bacterial colonization. You need:
- Accurate diagnosis: Comprehensive periodontal examination and oral microbiome testing
- Targeted treatment: Addressing specific pathogens, not just visible plaque
- Monitoring: Regular reassessment to ensure bacterial populations remain balanced
- Integration: Coordinating with your medical providers about your oral-systemic health risks
This isn't about creating fear — it's about empowering you with information.
Most people brush their teeth to prevent cavities and avoid bad breath. Few realize they're also maintaining a critical barrier against systemic disease.
What You Can Do Today
If you have any of these warning signs, comprehensive oral health assessment should be a priority:
- Bleeding gums when brushing or flossing
- Persistent bad breath despite good hygiene
- Gum recession or teeth appearing longer
- Loose teeth or changes in bite
- History of periodontal disease in your family
- Existing cardiovascular disease or risk factors
The Gateway to Health docuseries explores these connections in depth, featuring leading experts in both dentistry and cardiology.
You can watch the first episode free for 10 days and discover exactly how oral health influences every system in your body.
But watching alone won't change your health status. Testing will.
Knowing your specific oral microbiome composition gives you actionable data — the kind of information that allows for precise, personalized intervention.
Final Thoughts
The warning sign your dentist sees — chronic gum inflammation, pathogenic bacterial colonization, periodontal disease — isn't just about saving your teeth.
It's about protecting your heart, your brain, your entire cardiovascular system.
We've moved far beyond the old wisdom of "floss or die."
Now we understand the specific mechanisms: how bacteria travel from mouth to arteries, how chronic inflammation damages blood vessels, how oral pathogens destabilize arterial plaques.
We have the science. We have the testing technology.
What we need is for people to recognize that oral health IS cardiovascular health.
Your mouth is talking. Your gums are signaling. The question is: are you listening?
Sources
- Signal Transduction and Targeted Therapy. (2025). Porphyromonas gingivalis aggravates atherosclerotic plaque instability by promoting lipid-laden macrophage necroptosis.
- Frontiers in Immunology. (2023). Porphyromonas gingivalis regulates atherosclerosis through an immune pathway.
- Atherosclerosis. (2012). Porphyromonas gingivalis accelerates inflammatory atherosclerosis in the innominate artery of ApoE deficient mice.
- Frontiers in Immunology. (2021). Serum C-Reactive Protein and Periodontitis: A systematic review and meta-analysis.
- International Journal of Oral Science. (2023). Oral pathogen aggravates atherosclerosis by inducing smooth muscle cell apoptosis and repressing macrophage efferocytosis.
- Frontiers in Cardiovascular Medicine. (2023). Periodontal disease is associated with the risk of cardiovascular disease independent of sex: A meta-analysis.
- Journal of Clinical & Diagnostic Research. (2014). C-Reactive Protein (CRP) and its Association with Periodontal Disease: A Brief Review.
- PLOS One. (2014). Active invasion of oral and aortic tissues by Porphyromonas gingivalis in mice causally links periodontitis and atherosclerosis.
- Circulation. (2016). Periodontitis increases the risk of a first myocardial infarction.
- Global Heart. (2020). Periodontitis and cardiovascular diseases: Consensus report.
- Journal of Indian Society and Peridontology. (2010). The link between periodontal disease and cardiovascular disease: How far we have come in last two decades?
- Circulation. (2012). Periodontal disease and atherosclerotic vascular disease: Does the evidence support an independent association? American Heart Association Scientific Statement.
- npj Biofilms and Microbiomes. (2025). The oral-gut microbiota axis: a link in cardiometabolic diseases.
- Molecular Oral Microbiology. (2016). Effect of salivary agglutination on oral streptococcal clearance by human polymorphonuclear neutrophil granulocytes.
- Journal of Oral Microbiology. (2019). Can oral bacteria affect the microbiome of the gut?
- Microorganisms. (2024). Oral Microbiome: A Review of Its Impact on Oral and Systemic Health.
- Journal of Oral Microbiology. (2017). Porphyromonas gingivalis is the most abundant species detected in coronary and femoral arteries.
Gateway to Health is the new health & wellness division of The Urban Monk. We've moved the health and life sciences content here and are leaving the personal development and mindfulness materials on theurbanmonk.com.
Disclaimer: This content is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Please consult a qualified healthcare professional before making changes to your health protocol.