Gum Disease and Dementia: Are Your Gums Stealing Memory?
Dec 12, 2025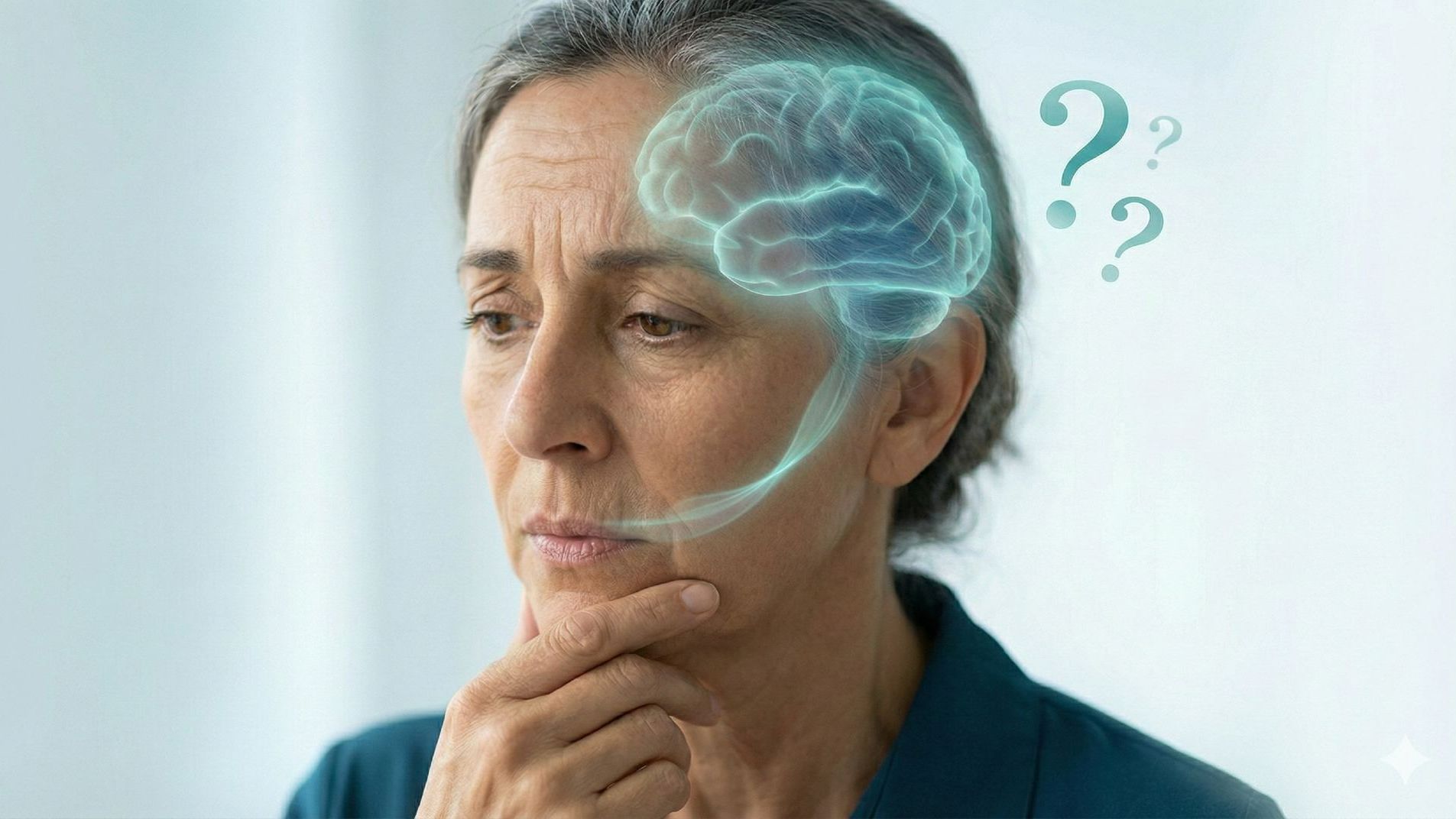
Gum disease and dementia: how bleeding gums could be the first warning sign of memory loss
You brush your teeth, notice a little blood in the sink, and think nothing of it. After all, your gums have bled for years.
But here's what conventional dentistry won't tell you: that blood could be carrying something far more dangerous than you realize — bacteria that travel straight to your brain.
The connection between gum disease and dementia isn't just emerging science anymore. It's an established fact.
Recent studies have found specific oral bacteria in the brains of Alzheimer's patients¹, and elevated antibodies against periodontal bacteria have been associated with increased risk of developing dementia².
In this article, you'll discover exactly how oral bacteria infiltrate your brain, which specific pathogens are most dangerous, and most importantly, what you can do right now to protect your cognitive health.
I'll walk through the science in plain terms and show you how testing your oral microbiome could be the most important health decision you make this year.
If you're experiencing bleeding gums, memory issues, or simply want to understand your oral-brain connection better, keep reading. There's critical information ahead that could change everything.
Key Takeaways
- People with severe gum disease have a 20% increased risk of developing dementia, while those with complete tooth loss have approximately twice the risk compared to those with healthy gums³, with specific oral bacteria found in Alzheimer's patients' brains.¹
- Two pathogens — Porphyromonas gingivalis and Fusobacterium nucleatum — can cross the blood-brain barrier and trigger neuroinflammation.⁴,⁵
- Bleeding gums aren't "normal" — they're entry points for bacteria into your bloodstream.
- Tooth loss accelerates brain atrophy, with each lost tooth increasing cognitive decline risk by 9-12% over time.⁶
- The oral-gut-brain axis means mouth bacteria affect both digestive health and cognitive function simultaneously.²,⁴
- Chronic gum inflammation produces the same inflammatory markers found in dementia patients.⁷
- Oral microbiome testing reveals which bacteria are in your mouth before symptoms become irreversible.
Discover the Mouth-Brain Connection
See how oral bacteria trigger the cascade of events leading to cognitive decline. Watch the complete Gateway to Health documentary series and understand the oral-systemic connections your dentist never explained.
The Bacteria Living in Your Mouth Right Now
Your mouth harbors over 700 species of bacteria. Most are harmless. Some are beneficial.
But a few are wreaking havoc you can't see.
When I review oral microbiome test results, I often see patients shocked by what's growing in their mouths.
They brush twice daily, floss regularly, see their dentist — and still test positive for dangerous pathogens linked to brain inflammation.
Here's the reality: conventional dental cleanings don't address the bacterial imbalances that drive systemic disease.
They remove surface plaque, but they don't rebalance your oral ecosystem.
And that ecosystem matters more than most people realize, especially when it comes to cognitive health and dementia risk.
The two bacteria we're most concerned about are Porphyromonas gingivalis (P. gingivalis) and Fusobacterium nucleatum (F. nucleatum).
The Two Most Dangerous Bacteria
Found in Alzheimer's patients' brains
Porphyromonas gingivalis
🔑 What It Does:
Produces gingipain enzymes that break down the blood-brain barrier9
⚠️ The Danger:
Directly triggers amyloid-beta plaque formation in brain tissue1
Fusobacterium nucleatum
🔑 What It Does:
Generates massive systemic inflammation throughout the body4
⚠️ The Danger:
Found in brain tissue and weakens protective barriers4,5
Both bacteria can be detected through oral microbiome testing before they cause irreversible brain damage.
Both have been found in the brain tissue of Alzheimer's patients⁴,⁵.
Both produce enzymes that break down brain cells. And both enter your bloodstream every time your gums bleed.⁷
Which Bacteria Are Living in Your Mouth Right Now?
Stop guessing and start knowing. Get your oral microbiome tested and discover your personalized protocol before dangerous pathogens like P. gingivalis compromise your cognitive health.
How Oral Bacteria Reach Your Brain
The pathway from mouth to brain is disturbingly direct.
When you have periodontal disease, your gums become inflamed and bleed easily⁸.
Each time they bleed — whether from brushing, flossing, or eating — bacteria enter your bloodstream through those tiny wounds.
This is called bacteremia, and it happens constantly in people with gum disease.
Once in your bloodstream, these bacteria face a critical barrier: the blood-brain barrier, which normally protects your brain from pathogens.
The Pathway: From Gums to Brain
Gum Inflammation & Bleeding
Periodontal disease creates wounds where bacteria enter bloodstream8
Bacteremia
Oral bacteria travel through bloodstream every time gums bleed7
Blood-Brain Barrier Breach
Gingipain enzymes degrade protective barrier, allowing bacteria into brain9
Neuroinflammation
Microglia immune cells activate to fight infection in brain tissue
Amyloid-Beta Plaque Formation
Brain produces Alzheimer's-defining plaques in response to bacterial infection1
⚠️ This cascade happens repeatedly with chronic gum disease — every time your gums bleed, bacteria enter your bloodstream.
But here's where it gets concerning: P. gingivalis produces enzymes called gingipains that can actually degrade this protective barrier⁹.
Think of it like bacteria carrying tiny keys that unlock your brain's security system.
F. nucleatum works differently but just as dangerously. It generates massive systemic inflammation that weakens the blood-brain barrier over time.⁴,⁵
Once these bacteria cross into brain tissue, they trigger an immune response that was never meant to happen there.
Your brain's immune cells, called microglia, go into overdrive trying to fight the infection.
But in their frenzy, they start producing amyloid-beta proteins — the same plaques that define Alzheimer's disease.¹
What started as a gum infection has now become neuroinflammation, and your brain is caught in friendly fire.
This isn't theoretical. Researchers have traced P. gingivalis DNA directly from infected gums to brain lesions in dementia patients¹.
The connection is no longer in question. The only question is whether it's happening in your mouth right now.
Don't Wait Until Symptoms Appear
Test your oral microbiome today and know exactly which bacteria are present before they cross the blood-brain barrier and trigger neuroinflammation.
Once bacteria reach your brain, the damage compounds over time. Early detection gives you the power to intervene before cognitive decline begins.
The Inflammation Connection
If bacteria were the only problem, this would be simpler.
But gum disease creates something more insidious: chronic low-grade inflammation that spreads throughout your entire body.
When your gums are inflamed, they continuously release inflammatory molecules — cytokines like IL-6, IL-1β, and TNF-α — into your bloodstream⁷.
These same molecules are elevated in Alzheimer's patients. They're not just markers of disease; they're active participants in brain deterioration.
This chronic inflammatory state affects your brain in multiple ways.
It accelerates the breakdown of the hippocampus, the brain region responsible for memory formation¹⁰.
It promotes the accumulation of those amyloid-beta plaques we mentioned.
And it interferes with your brain's ability to clear out cellular waste, essentially creating a toxic environment where neurons struggle to survive.
One patient recently told me her gums had bled for decades. She'd mentioned it to multiple dentists, but they just told her to floss more.
When we finally tested her oral microbiome, she had dangerous levels of P. gingivalis. Within weeks of following her personalized protocol, the bleeding stopped.
More importantly, the brain fog she'd experienced for years started to lift.
The inflammatory connection extends beyond just your brain.
Studies show that periodontal disease and dementia risk overlaps significantly with cardiovascular disease and diabetes²,¹² — all conditions driven by chronic inflammation.
Your mouth isn't just connected to your brain. It's connected to every system in your body.
It's Not Just Your Brain
Oral inflammation affects your entire body
Watch the complete Gateway to Health series and discover how oral inflammation connects to your heart, gut, and brain — the full-body connections most people never learn about.
Tooth Loss and Brain Atrophy
Here's something that surprised even me when I first encountered the research: every tooth you lose accelerates brain shrinkage.
A prospective study following older men for over 32 years found that each tooth lost per decade increased the risk of cognitive decline by 9-12%.⁶
Think about that.
Not "might increase."
Not "could potentially increase."
Actually increases, measurably, year after year.
Why? Several mechanisms appear to be at work.
Tooth Loss = Brain Shrinkage
The connection is measurable and significant
9-12%
increased cognitive decline risk per tooth lost per decade
Source: 32-year prospective study6
Nutritional Deficiencies
Difficulty chewing leads to avoiding nutrient-dense foods critical for brain health11
Reduced Brain Stimulation
Chewing increases blood flow to the brain and activates memory regions11
Years of Bacterial Exposure
Tooth loss typically follows chronic periodontal infection, meaning bacteria have repeatedly seeded brain tissue10
📊 MRI studies show visible gray matter atrophy in the hippocampus of people with significant tooth loss6,10
First, tooth loss changes how you eat.
You start avoiding harder-to-chew foods — often the nutrient-dense vegetables and proteins your brain needs¹¹.
Nutritional deficiencies follow, particularly B vitamins crucial for cognitive function.
Second, tooth loss reduces what researchers call "masticatory function" — the act of chewing itself.
This might seem trivial, but chewing stimulates blood flow to your brain. It activates specific brain regions involved in memory¹¹.
When you lose teeth and stop chewing effectively, you're literally reducing the stimulation your brain receives.
Third, and perhaps most critically, tooth loss is usually the end result of severe periodontal disease.
By the time teeth are lost, chronic infection and inflammation have often persisted for years — plenty of time for oral bacteria to repeatedly seed your brain tissue.
MRI studies have confirmed this visually.
People with significant tooth loss show measurable gray matter atrophy in the hippocampus and other memory-critical brain regions¹⁰.
The brain literally shrinks in response to the cascade of events triggered by oral disease.
Why Testing Matters More Than Guessing
I can't see what's in your mouth just by looking. Neither can your dentist. Surface examinations miss the microbial reality underneath.
Signs You Need Oral Microbiome Testing
Don't wait for symptoms to become irreversible
Bleeding gums when brushing or flossing
Recurrent cavities despite good oral hygiene
Memory issues or brain fog
Persistent bad breath that doesn't improve
Family history of dementia or Alzheimer's
Gum recession or tooth loss
💡 Testing reveals which bacteria are present before they cause irreversible damage to your brain health
This is where oral microbiome testing becomes essential.
A comprehensive test identifies not just whether harmful bacteria are present, but in what quantities, which species dominate, and how balanced — or imbalanced — your oral ecosystem has become.
One patient came to me frustrated after years of recurring cavities despite excellent oral hygiene.
Her dentist kept filling cavities but never addressed why they kept forming.
When we tested her oral microbiome, we found she had extremely high levels of Streptococcus mutans (the main cavity-causing bacteria) alongside elevated P. gingivalis.
Her personalized protocol addressed both issues simultaneously.
Within three months, her cavities stopped forming. Her gums stopped bleeding.
And she reported feeling more mentally sharp than she had in years — a benefit she hadn't even been seeking.
Testing removes the guesswork.
Instead of trying random solutions — different toothpastes, mouthwashes, supplements — you get targeted interventions based on your actual bacterial profile.
You know exactly which pathogens need to be addressed and which beneficial species need support.
The oral microbiome testing we use identifies key bacterial species, including the specific pathogens linked to dementia risk.
You'll see precisely what's growing in your mouth and what it means for your long-term brain health.
Discover Which Bacteria Are Affecting Your Cognitive Health
Take the Orobiome Test and receive a personalized protocol based on your unique bacterial profile.
What You Can Do Starting Today
Understanding the connection between oral health and cognitive decline is step one.
Taking action is where real protection begins.
First, pay attention to bleeding gums.
I don't care what you've been told — bleeding gums are never normal.
They're a red flag that your oral microbiome is out of balance and bacteria are entering your bloodstream.
If you see blood when you brush, that's your body's alarm system going off.
Second, consider your current oral care routine.
Most commercial mouthwashes kill everything in your mouth — good bacteria and bad — creating an ecological disaster that harmful species exploit.
The leaky mouth syndrome we see so often starts with well-intentioned but misguided oral care.
Third, understand that what happens in your mouth affects your gut, and what happens in your gut affects your brain.
These systems aren't separate. They're intimately connected through what we call the oral-gut-brain axis. Supporting one supports them all.
I recently had a patient tell me something that stuck with me.
She said, "I spent years trying to fix my memory with supplements and brain games. Nobody ever told me to start with my teeth."
After addressing her periodontal disease and rebalancing her oral microbiome, her cognitive symptoms improved more than they had with any other intervention.
That's not uncommon.
When we remove chronic bacterial infections and calm systemic inflammation, the brain has room to heal.
But you have to address the source, not just manage symptoms.
The most effective approach starts with comprehensive testing.
Know what you're dealing with. Then build a personalized protocol that targets your specific imbalances.
That's functional oral health, and it's how we protect not just your teeth but your brain.
Ready to Protect Your Cognitive Health?
Get testing + personalized protocol designed for YOU
Get your oral microbiome tested and receive a personalized protocol designed specifically for your unique bacterial profile — before dangerous pathogens compromise your brain health.
What's Included:
Your Brain Depends on Your Mouth
The science is clear: gum disease and dementia are connected through mechanisms we can now trace, measure, and most importantly, address.
Oral bacteria don't stay in your mouth. They travel. They cross barriers. They trigger inflammation that reaches your brain.
But here's the hopeful part — this connection works both ways.
Improving your oral health can reduce your dementia risk.
Rebalancing your oral microbiome can lower brain inflammation.
Addressing periodontal disease now can protect your cognitive function for decades to come.
You don't have to accept bleeding gums as normal.
You don't have to watch your memory fade and wonder if there was something you could have done.
And you certainly don't have to keep guessing about what's happening in your mouth while dangerous bacteria multiply unchecked.
Testing reveals the truth. Targeted protocols create change. And protecting your oral health today protects your brain for tomorrow.
Stop guessing. Start testing. Your memory depends on it.
Stop Guessing. Start Protecting Your Brain.
Get tested today and receive your personalized protocol from our team of functional dentists
You'll know exactly which bacteria are in your mouth, what they mean for your cognitive health, and the specific steps to rebalance your oral ecosystem before damage becomes irreversible.
Your Complete Package Includes:
Your memory depends on what's happening in your mouth right now.
Sources
- Porphyromonas gingivalis in Alzheimer's disease brains: Evidence for disease causation and treatment with small-molecule inhibitors. Science Advances. 2019.
- Clinical and bacterial markers of periodontitis and their association with incident all-cause and Alzheimer's disease dementia in a large national survey. Journal of Alzheimer's Disease. 2020.
- Are Your Gums Saying Something About Your Dementia Risk? American Academy of Neurology. 2020.
- Fusobacterium nucleatum reduces METTL3-mediated m6A modification and contributes to colorectal cancer metastasis. Nature Communications. 2022.
- Periodontal Disease and Alzheimer's: Insights from a Systematic Literature Network Analysis. The Journal of Prevention of Alzheimer’s Disease. 2024.
- Association between adverse oral conditions and cognitive impairment: A literature review. Frontiers in Public Health. 2023.
- Cytokines in gingivitis and periodontitis: from pathogenesis to therapeutic targets. Frontiers in Immunology. 2024.
- About Periodontal (Gum) Disease. CDC Oral Health. 2024.
- Good oral health may help protect against Alzheimer’s. Harvard Medical School. 2019.
- Associations of Dental Health With the Progression of Hippocampal Atrophy in Community-Dwelling Individuals. Neurology. 2023.
- Relationship of tooth loss to mild memory impairment and cognitive impairment: Findings from the Fujiwara-kyo Study. Behavioral and Brain Functions. 2010.
- Increased cardiovascular risk in people with type 2 diabetes and periodontitis: an analysis from a global real-world federated database. British Dental Journal. 2025.
Gateway to Health is the new health & wellness division of The Urban Monk. We've moved the health and life sciences content here and are leaving the personal development and mindfulness materials on theurbanmonk.com.
Disclaimer: This content is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Please consult a qualified healthcare professional before making changes to your health protocol.