Oral Bacteria and Gut Health: A Dentist's Warning
Dec 25, 2025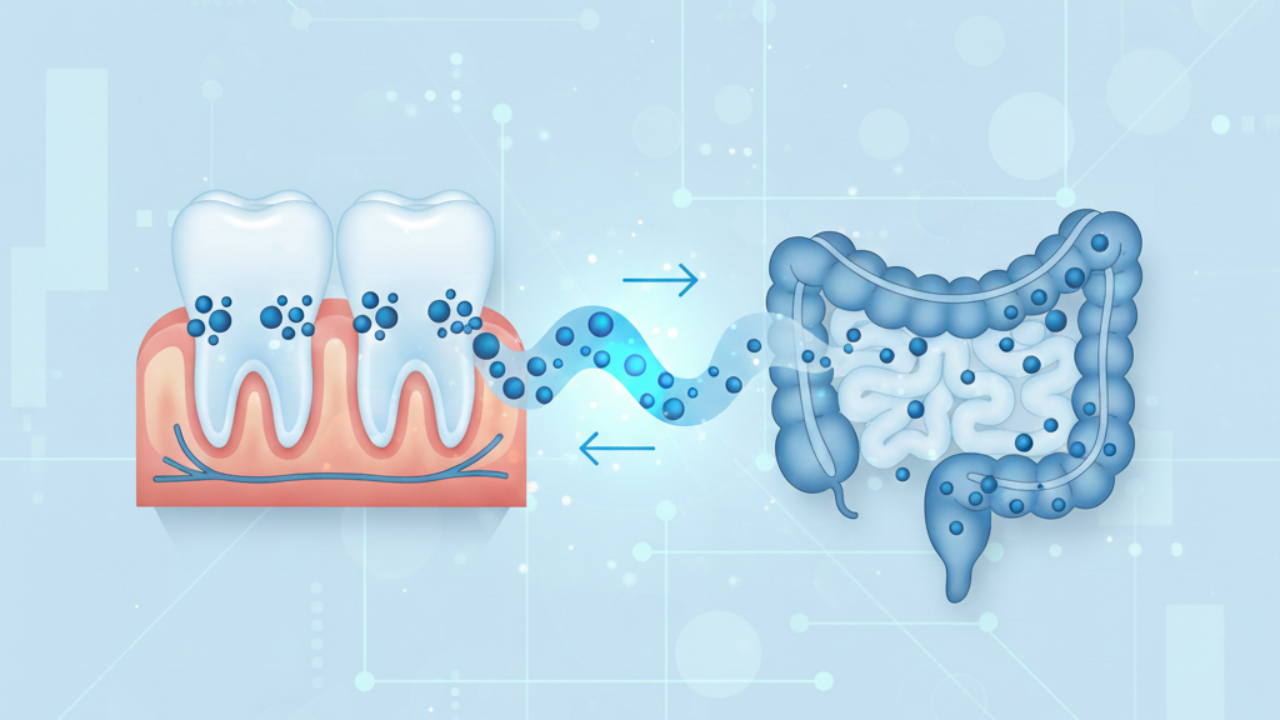
Oral Bacteria and Gut Health: What Functional Dentistry Taught Me About the Mouth-Gut Axis
Throughout my 18 years of clinical dentistry practice, I saw countless patients who'd spent years chasing gut health solutions — eliminating foods, taking supplements, following strict protocols — yet their digestive issues persisted.
When I examined their mouths, I often found the answer: chronic gum inflammation, bleeding tissue, and an oral microbiome completely out of balance.
The connection between oral bacteria and gut health isn't just important — it's fundamental to understanding why your digestive system isn't healing.
In this article, you'll discover how mouth bacteria directly influence your gut microbiome and what comprehensive testing reveals that conventional approaches miss.
If you've been struggling with gut issues despite doing "everything right," the information ahead could be your turning point.
Discover the Oral-Systemic Connection
Your mouth affects more than your teeth — it influences your gut, brain, heart, and entire body. Watch the Gateway to Health docuseries FREE for 10 days and discover the oral-systemic connections that could transform your health.
✓ 10 days of free access • ✓ New episodes unlock daily • ✓ Expert-led education
Key Takeaways
- You swallow approximately 100 billion oral bacteria daily¹ that directly seed your intestinal tract and can dramatically alter gut microbiome composition².
- Pathogenic oral bacteria like Porphyromonas gingivalis disrupt intestinal tight junction proteins, creating "leaky gut" and systemic inflammation²,⁶.
- The oral-gut connection operates bidirectionally — oral dysbiosis affects digestive health, while gut inflammation can worsen periodontal disease³,¹⁴.
- Bleeding gums aren't just a dental problem — they're a direct pathway for harmful bacteria to enter your bloodstream and colonize your digestive tract⁷,⁸.
- Addressing oral bacteria reduces inflammatory markers throughout the body, including the gut, where chronic inflammation drives most digestive disorders¹¹,¹⁵.
- Traditional gut health programs that ignore the mouth miss a critical source of ongoing dysbiosis and reinfection.
- Comprehensive oral microbiome testing reveals which specific bacteria are disrupting your gut healing — guessing doesn't work.
Which Bacteria Are Affecting YOUR Gut?
Orobiome testing identifies exactly which oral pathogens are present in your mouth — giving you the personalized roadmap to address oral dysbiosis before it continues sabotaging your digestive healing.
✓ At-home test (under 5 minutes) • ✓ DNA-level analysis • ✓ Personalized protocol included
Understanding the Mouth-Gut Axis
Pivoting to functional dentistry taught me something that still surprises most people: your mouth and your gut aren't separate systems.
They're directly connected by what researchers call the "oral-gut axis."
You produce approximately 0.5 to 1.5 liters of saliva daily,³ containing about 100 million bacteria per milliliter.⁴
Every time you swallow, you're sending those microorganisms into your digestive system — researchers estimate we swallow up to 100 billion bacteria every 24 hours.¹
In a healthy mouth, this bacterial flow supports gut function.
But when your oral microbiome is dysbiotic — from gum disease, chronic inflammation, or bacterial imbalance — you're seeding your gut with inflammatory organisms multiple times per hour, every single day.
One patient I worked with had followed an elimination diet for two years with minimal improvement.
Within six weeks of treating her periodontal disease and rebalancing her oral microbiome, her bloating decreased by 70% and food sensitivities began resolving.
The mouth-gut connection explained what years of random gut-focused treatments couldn't.
See the Science Behind the Oral-Gut Axis
This isn't just theory — it's documented clinical reality. The Gateway to Health docuseries explores these connections in depth, showing you exactly how oral bacteria migrate to your gut and what you can do about it.
✓ 10 days of free access • ✓ New episodes unlock daily • ✓ Evidence-based education
How Oral Bacteria Colonize Your Digestive System
The journey from mouth to gut happens through three pathways.
The enteral route is most direct: bacteria travel with food and saliva into your gastrointestinal tract.⁵
While stomach acid usually prevents colonization, compromised gut barrier function allows oral bacteria to establish themselves.
Research in PLOS One found that P. gingivalis administration altered gut microbiota and downregulated tight junction proteins like ZO-1 and occludin² — proteins that seal intestinal cells and prevent "leaky gut."
The hematogenous route is more concerning.
With bleeding gums — affecting approximately 47% of adults aged 30 and older⁷ — oral bacteria enter your bloodstream during brushing or chewing.
A review in Trends in Cardiovascular Medicine documented how bacterial translocation triggers systemic inflammation affecting the entire digestive system.⁸
The immune cell migration route allows oral bacteria to survive inside immune cells and travel from oral mucosa to intestinal lining,⁹ explaining why addressing oral health improves gut conditions even when oral bacteria aren't detected in stool.
3 Ways Oral Bacteria Colonize Your Gut
Every swallow sends bacteria from your mouth into your body through these pathways
1. The Enteral Route
Bacteria travel directly with food and saliva into your digestive tract. When gut barriers are compromised, oral pathogens establish colonies and disrupt intestinal health.
2. The Hematogenous Route
Bleeding gums create entry points for bacteria to enter your bloodstream during brushing or chewing. This triggers systemic inflammation affecting your entire digestive system.
3. Immune Cell Migration
Oral bacteria survive inside immune cells and travel from oral tissues to intestinal lining — explaining why addressing oral health improves gut conditions even when oral bacteria aren't detected in stool.
The Bacteria That Do the Most Damage
Not all oral bacteria affect gut health equally.
Through clinical experience and research on oral pathogens, certain species are particularly destructive.
Porphyromonas gingivalis is the most well-studied periodontal pathogen.
When it reaches the gut, it acts as a keystone species — even at low levels, dramatically shifting the entire gut microbiome toward disease.¹⁰
Studies show P. gingivalis leads to decreased gut diversity, increased intestinal permeability, and elevated inflammation.¹¹
The mechanism: it produces enzymes called gingipains that directly degrade tight junction proteins.¹²
One patient I worked with had inflammatory bowel disease. Her oral microbiome test revealed elevated P. gingivalis levels.
After targeted treatment, her inflammatory markers improved more than with any gut-focused intervention alone.
Fusobacterium nucleatum is another problematic oral bacterium.
A new study published in NPJ Biofilms and Microbes found that:
“F. nucleatum may promote inflammation and disease progression by modulating host immune responses and destabilizing the intestinal microenvironment”.¹³
The researchers also noted that:
“Recent studies have further implicated Fusobacterium in functional gastrointestinal disorders, such as irritable bowel syndrome (IBS) and functional dyspepsia.”¹³
These bacteria don't just cause direct damage — they shift your intestinal microbiome toward inflammatory species while suppressing beneficial bacteria, creating a self-perpetuating cycle.
Are These Pathogens in YOUR Mouth?
P. gingivalis and F. nucleatum could be colonizing your oral microbiome right now. Explore the Orobiome Test to identify exactly which species need addressing before they continue disrupting your digestive health.
✓ Detects harmful bacteria • ✓ Species-level identification • ✓ Licensed dentist review
When Gut Health Affects Your Mouth
The oral-gut connection works both ways.
Gut dysbiosis doesn't just result from oral bacteria — it worsens periodontal disease.
Studies show gut inflammation alters oral microbiome composition through systemic inflammatory mediators.¹⁴
When your gut barrier is compromised, bacterial endotoxins trigger immune responses affecting your gums.
The Vicious Cycle
Dysfunction in one system perpetuates problems in the other
Oral Dysbiosis → Gut Inflammation
Pathogenic oral bacteria migrate to your gut, disrupting intestinal barrier function and triggering chronic digestive inflammation.
Gut Dysbiosis → Periodontal Disease
Compromised gut barriers release inflammatory cytokines (TNF-α, IL-6) into your bloodstream, making gums more susceptible to infection.
💡 Key Insight: You can't heal one system while ignoring the other — both must be addressed for lasting results.
Gut dysbiosis increases inflammatory cytokines like TNF-α and IL-6,¹⁵ which travel through your bloodstream making gums more susceptible to infection.
I treated patients whose periodontal disease improved when we addressed gut health, and others whose digestive symptoms resolved when we treated gum disease.
One patient told me, "I feel like I've been fighting both ends of the same battle without realizing they were connected."
Once we coordinated care and addressed the oral-gut axis as one system, both conditions improved dramatically.
Your Body is One Connected System
Understanding the gut-brain-immune-hormonal connection changes everything. Watch Interconnected FREE for a limited time and discover how healing one system transforms them all.
✓ Limited-time free access • ✓ Systems-based approach • ✓ Transform your health
Why Your Gut Won't Heal Until You Address Your Mouth
If you have periodontal disease or oral dysbiosis, your gut healing will be incomplete at best.
You can follow perfect gut protocols, but if you're swallowing billions of pathogenic bacteria daily, you're constantly reinfecting your gut.
Research shows individuals with periodontal disease have significantly less diverse gut microbiomes and higher inflammatory oral species throughout their intestines.¹⁶
I saw this repeatedly — patients tried multiple gut protocols with minimal success. We tested their oral microbiome and found significant dysbiosis.
After addressing it, gut symptoms improved more in weeks than months of gut-focused interventions.
You can't heal an ecosystem while actively poisoning it with upstream pathogens.
Understanding holistic dental care means recognizing your mouth is the beginning of your digestive system — not a separate entity.
Stop Treating Symptoms. Address the Source.
If you're constantly reinfecting your gut with oral bacteria, no protocol will work. Orobiome testing reveals exactly which bacteria are sabotaging your healing efforts — so you can finally address the root cause instead of endlessly treating symptoms.
✓ Find the root cause • ✓ Stop the reinfection cycle • ✓ Targeted protocol included
Testing Reveals What Guessing Misses
Throughout my clinical years, conventional approaches involved guessing rather than measuring.
Traditional dentistry looks for cavities but rarely assesses the oral microbiome.
Gut protocols recommend broad interventions without knowing specific imbalances.
After watching patients struggle, I became convinced comprehensive testing is the only way to understand your oral-gut axis — why we developed Gateway to Health's testing-first approach.
Oral microbiome testing identifies pathogenic species like P. gingivalis and F. nucleatum, beneficial bacteria balance, inflammatory markers, and ecosystem stability.
This tells us exactly which interventions to prioritize — targeted antimicrobials, probiotic restoration, or both in specific sequences.
One patient had tried random treatments for her gut for three years unsuccessfully.
Her oral microbiome test revealed three pathogenic species and absent protective bacteria. We designed a protocol targeting oral dysbiosis while supporting her gut.
Within two months, decade-long digestive issues began resolving. Oral microbiome testing provides the roadmap for healing.
Guessing vs. Knowing: Years of Difference
The difference between guessing and measuring can mean years of unnecessary suffering. Get your Orobiome test and discover exactly which bacteria are preventing your gut from healing.
✓ Precision testing • ✓ Clear answers, not guesses • ✓ Personalized roadmap
The Complete Picture: Testing Both Ends of the Axis
For the most comprehensive understanding of what's happening in your oral-gut axis, testing both ends of this critical pathway reveals patterns that single-system testing misses.
Start with your oral microbiome.
Orobiome testing identifies which specific oral bacteria are present, their levels, and whether pathogenic species like P. gingivalis or F. nucleatum are colonizing your mouth.
This shows you exactly what's being swallowed into your digestive tract every single day.
Then assess your gut.
Comprehensive gut testing reveals whether oral pathogens have established themselves in your intestines, how they're affecting your gut microbiome diversity, and whether your intestinal barrier function is compromised.
This testing shows the downstream effects of oral dysbiosis.
Together, these tests answer critical questions:
- Are oral bacteria driving your gut problems?
- Is gut inflammation worsening your oral health?
- Are you caught in a vicious cycle where dysfunction in both systems perpetuates the other?
One patient I worked with had SIBO, leaky gut, and food sensitivities. Her practitioners focused exclusively on the gut.
When we tested both her oral and gut microbiomes, we found two oral pathogens at high levels in both locations.
Addressing the oral source first allowed her gut bacterial overgrowth to resolve faster than gut-directed treatments alone ever achieved.
By testing both systems, you create a personalized, root-cause protocol rather than following generic templates that ignore half the equation.
Moving Forward: An Integrated Approach
My experience in both clinical and functional dentistry has shown me that oral and gut health are inseparable.
The evidence is overwhelming: oral bacteria directly influence gut microbiome composition, intestinal barrier function, and systemic inflammation.
If you're struggling with unresolved gut issues, consider whether your mouth is the missing piece.
Look for signs: bleeding gums, chronic bad breath, frequent cavities, gum recession, visible inflammation.
These aren't just dental concerns — they're red flags that pathogenic bacteria may be flowing into your gut with every swallow.
Addressing oral-gut dysfunction is entirely possible with proper testing and targeted interventions.
Through Gateway to Health, we provide online consultations and suggest protocols that collaborate with your clinical dentist to create comprehensive protocols.
Our Gateway to Health series offers 10 days of free viewing with comprehensive education on how oral health influences your entire body, including detailed episodes on the mouth-gut connection.
For those ready to act, start with Orobiome testing to identify which oral bacteria are disrupting your health, then follow with comprehensive gut testing to see the full picture of how these systems interact.
Together, these tests provide the roadmap for true, lasting healing.
Your mouth is the gateway to your gut, and your gut is the gateway to overall health.
After watching patients finally resolve chronic digestive issues by addressing this connection: you can't afford to ignore it any longer.
Sources
- A practical guide to the oral microbiome and its relation to health and disease. Oral Diseases. 2018.
- Oral administration of P. gingivalis induces dysbiosis of gut microbiota and impaired barrier function leading to dissemination of enterobacteria to the liver. PLOS One. 2015.
- Saliva and gastrointestinal functions of taste, mastication, swallowing and digestion. Oral Dis. 2002.
- Multispecies communities: interspecies interactions influence growth on saliva as sole nutritional source. Int J Oral Sci. 2011.
- The bacterial connection between the oral cavity and the gut diseases. J Dent Res. 2020.
- Porphyromonas gingivalis indirectly elicits intestinal inflammation by altering the gut microbiota and disrupting epithelial barrier function through IL9-producing CD4+ T cells. Mol Oral Microbiol. 2022.
- Periodontal Disease in Adults (Age 30 or Older). National Institute of Dental and Craniofacial Research. 2021.
- Detection of periodontal microorganisms in coronary atheromatous plaque specimens of myocardial infarction patients: a systematic review and meta-analysis. Trends Cardiovasc Med. 2021.
- Multifaceted impacts of periodontal pathogens in disorders of the intestinal barrier. Front Immunol. 2021.
- Roles of Porphyromonas gingivalis and its virulence factors in periodontitis. Adv Protein Chem Struct Biol. 2021.
- Oral administration of Porphyromonas gingivalis alters the gut microbiome and serum metabolome. mSphere. 2018.
- Porphyromonas gingivalis: An overview of periodontopathic pathogens below the gum line. Front Microbiol. 2016.
- Fusobacterium in the microbiome: from health to disease across the oral–gut axis and beyond. Npj Biofilms and Microbes. 2025.
- Genetic evidence strengthens the bidirectional connection between gut microbiota and periodontitis: insights from a two-sample Mendelian randomization study. J Transl Med. 2023.
- Immunological mechanisms of inflammatory diseases caused by gut microbiota dysbiosis: A review. Biomedicine & Pharmacotherapy. 2023.
- Defining the gut microbiota in individuals with periodontal diseases: an exploratory study. J Oral Microbiol. 2018.
Gateway to Health is the new health & wellness division of The Urban Monk. We've moved the health and life sciences content here and are leaving the personal development and mindfulness materials on theurbanmonk.com.
Disclaimer: This content is for educational purposes only and is not intended to diagnose, treat, cure, or prevent any disease. Please consult a qualified healthcare professional before making changes to your health protocol.